His dentist may have found it odd, but David Relman was walking in venerable footsteps when he arrived for his checkup 20 years ago with dry ice and a clutch of test tubes.
Three hundred years prior, a trailblazing Dutch lens-maker named Antonie van Leeuwenhoek had scrutinized a glob of his own plaque under a homemade microscope, marking humankind’s first sighting of the microbes teeming throughout our bodies.
Relman was about to do the same, though with awesome new firepower. Rather than just culturing samples in a petri dish, he adapted a process of rapid genetic sequencing from scientists exploring microbes in soil and water. Using the new method, Relman uncovered more than 30 bacterial species previously unseen.
But the bigger stunner would come in 2005, after Relman lowered his aim to the gut, this time revealing hundreds of unknown bacteria. And these bugs weren’t bit players. They included the most plentiful species in the large intestine, an “unseen majority” that was alive and well and, to that point, invisible in our bowels.
“The first thing I started thinking was, ‘Man, all these textbooks are completely, flat-out wrong,’ ” says Relman, a physician and professor of microbiology and immunology at the School of Medicine. “If you don’t know these things are here in health, in such numbers and presumably important, how do you even know when you’ve returned somebody to health?”

Other strange insights into our large intestines followed. In a milestone experiment, Professor Jeff Gordon’s lab at Washington University in St. Louis took mice with genetic mutations causing obesity and transferred their gut microbes to skinny brethren, who became fat themselves even though they lacked that mutation. The mechanics were murky, but one thing was clear: Our guts are home to a more diverse, more powerful population of outsiders than many had ever considered.
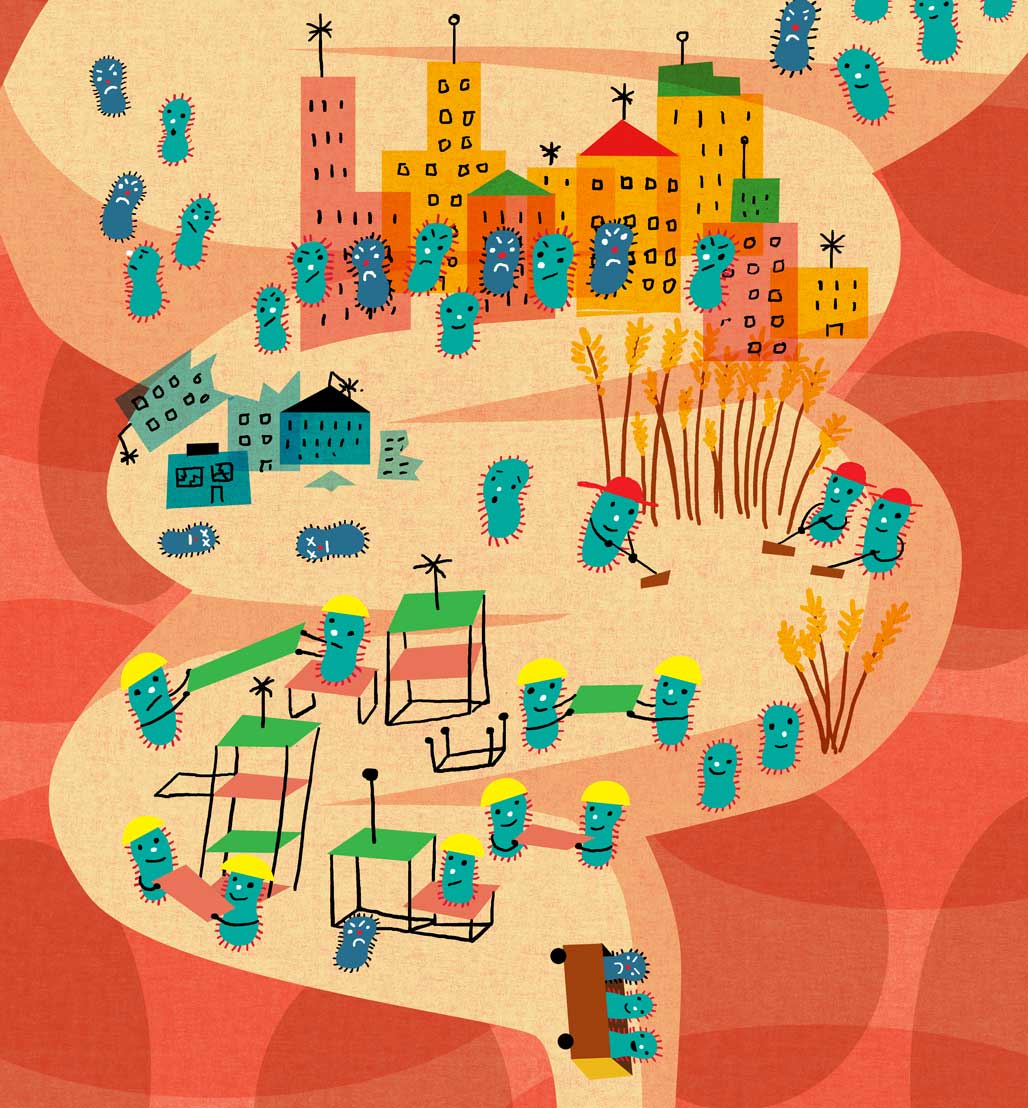
A dozen years later, the gut microbiome—as the community of viruses, fungi and, most populously, bacteria is dubbed—remains rife with mystery. It’s one thing to enumerate types of bacteria, another to know how they operate and interact in their ever-shifting trillions. But scientists at Stanford and elsewhere are pushing to fill in the details, drawn on by a tantalizing hope: the microbiome’s potential as a tunable “organ” whose influence could be tweaked to fight illness, maintain health and maximize performance.
“It’s malleable, unlike our human genome,” says Justin Sonnenburg, associate professor of microbiology and immunology at the School of Medicine, and co-leader with Relman of Stanford’s Center for Human Microbiome Studies. “That means if you’re getting ready to run a marathon versus getting ready to start immunotherapy for cancer, we might change your microbiome differently to tune your immune system or your metabolism to a different set point for the given situation.”
A New Look For Bacteria
Such grand hopes stand in contrast to the often unglamorous day-to-day science involved in microbiome research. The easiest way to study the gut, home to the densest collection of microbes in our bodies, is through our waste. By dry weight, human feces are 60 percent bacteria.

‘Sixteen years of college and you have to come out and pick up people’s poops. Maybe I will not send my kids to college anymore.’
Aashish Jha, a Stanford postdoc who worked with Sonnenburg on research in Nepal, recalls the bemusement of a woman who realized he was spending the day putting her fellow villagers’ donated stool into test tubes. “She asked, ‘Earlier, didn’t you say you went to college for 16 years?’ ” Jha says. “I said, ‘Yes,’ and she said, ‘Sixteen years of college and you have to come out and pick up people’s poops. Maybe I will not send my kids to college anymore.’ ”
But Jha, who used to feel disgust at seeing someone pick up after a dog, was unfazed. The research, he says, suggests that diverging lifestyles between foragers and people in agricultural communities have led their gut populations to diverge as well.
Newcomers usually get past any fecal phobia pretty quickly, says Ami Bhatt, an assistant professor of medicine and genetics, who is not the only microbiome researcher at Stanford to decorate her website with cartoonish poop icons. Behind that winking veneer, Bhatt has serious goals, including trying to use our bacterial co-travelers to help cancer patients avoid the potentially deadly side effects of stem-cell transplants.
It’s not a focus she could have anticipated when she started medical school in 1998. At that time, bacteria—at least those deemed worthy of scrutiny—were largely typecast as villains and marauders, as they had been since the late 19th century, when germ theory reformed notions that disease spread by deadly vapors. “We were very solidly trained in a kind of dogma that all bacteria you learn about are bad and most bacteria you can name are bad,” Bhatt says.
There were good reasons for the bias. Pathogens were responsible for millennia of misery. And the advent of antiseptic surgery, antibiotics, pasteurization and modern sanitation saved countless lives. Killer germs demanded our attention, and they got it.
It was only after reading Relman’s research that Bhatt says she began to reconsider the bacteria in the background. “The gears started turning,” she says. “Slowly I figured . . . they can’t all be pathogenic. Our model of most bacteria being bad for humans must be wrong—or at least limited.”
It’s a challenging shift in perspective, one that takes you away from the trees and to the sprawling forest. While a pathogen announces itself—it makes you sick—the wider bacterial community constitutes a vast, ever-morphing ecosystem in which cause and effect are far from obvious.
Today, Bhatt’s research seeks to capitalize on that more nuanced view. Working with a fragile population—leukemia and lymphoma patients who have received stem-cell transplants—Bhatt has been investigating the benefits of encouraging certain types of gut bacteria.
It’s a page out of Mother Nature’s book. For years, scientists were stumped as to why breast milk contains a complex sugar that a baby’s stomach can’t digest. The mystery lifted when they realized the compound fed beneficial bacteria in the colon, giving those strains a head start on colonizing a newborn’s pristine gut. In the womb, we’re mostly germ-free, but a microbial land rush begins upon exit. Breast milk tilts the odds in favor of a desirable neighbor taking root and crowding out pathogens.
In Bhatt’s case, she is looking for bacteria that could help reduce the mortality rate associated with stem-cell transplants. Around 30 percent of patients don’t survive the first year after transplant, she says. A third of that group succumbs to a return of the cancer, but the majority falls to ensuing complications, including intractable diarrhea and graft-versus-host disease, wherein the donor’s immune cells attack the recipient’s cells and microbiota.
The mortality problem, Bhatt says, may be exacerbated by damage to the patient’s microbiome caused by heavy doses of chemotherapy before the transplant. Studies have shown that the microbiome helps shape the immune system. In lab experiments, mice raised in microbe-free conditions develop compromised immune systems that never fully mature.
Scientists believe that immune cells and microbes are in constant dialogue. That communication may be imperiled once the chemo devastates the gut bacteria, causing the immune system to tip into self-sabotaging attack mode. “We know that low gut microbiome diversity in our bone marrow patients is associated with poor survival,” Bhatt says. “Maybe it’s just that we’re losing the microbes that produce signals that tell our immune system to chill out.”
In an early-stage experiment, with no reportable results as of yet, Bhatt’s lab has looked at the effects of giving patients doses of dietary fiber that are indigestible to the human body but that make fine dining for certain types of bacteria. In turn, these bacteria produce short-chain fatty acids, which give us energy, bolster our intestinal walls and may reduce inflammation associated with conditions ranging from irritable bowel syndrome to asthma to graft-versus-host disease. “We’re trying to feed the bugs that produce anti-inflammatory compounds,” she says.
Fiber For All
It’s not just the ill whose guts stand to benefit from increased fiber intake; it’s just about everybody on a typical American diet, according to Justin and Erica Sonnenburg, a husband-and-wife research team at the School of Medicine.
Our high-calorie, high-fat, low-fiber processed fare might be making us obese in record numbers, but it supplies nothing to our fiber-chomping microbiota. “We’re leaving our gut microbes starving,” Justin Sonnenburg says.
The potential consequences make the strain of constipation, the familiar bogeyman of the fiber-deprived, seem minor. Animal studies suggest that in the absence of fiber, mucus-eating microbes proliferate, consuming the protective coating of the large intestine and possibly inducing inflammation. According to the Sonnenburgs’ lab research, if the gut is deprived of fiber for too long, microbial species begin to die off and are not passed on to the next generation, resulting in ever-winnowing gut diversity.
This cycle may explain why people in Western nations have far fewer bacterial species in their gut than many of the world’s hunter-gatherer communities, whose fiber-heavy diets typify the way humanity lived for most of its existence.
A host of modern norms are also suspected in the microbiome’s plight. Lax use of broad-spectrum antibiotics kills off bacteria en masse; high C-section rates prevent passage through the microbe-rich birth canal; and strict, even obsessive, hygiene standards—“Hand sanitizer for everyone!”—reduce our exposure to all germs, not just the minority that might harm us.
It’s an open question what that means. Some say we’ve just ended up with microbiomes appropriate to our time and place, but the Sonnenburgs worry about a widening disconnect between our ancient, inflexible genome and our rapidly transforming microbiome. For tens of thousands of years, our genome and microbiome evolved together. Now that intimacy has been broken. It’s a concept the Sonnenburgs see encapsulated in a Los Angeles mural by the street artist Banksy that shows a caveman forlornly holding a tray with a burger, fries and a large drink.
Genetically, we’re not much different from Banksy’s caveman, yet we rely on a diet that’s unlike anything he, or his microbes, would recognize. The rapid change in our microbiome may explain the soaring number of allergies and Western diseases. Crohn’s disease, ulcerative colitis, diabetes and food allergies are largely unknown among populations like the Hadza, a foraging people in Tanzania that the Sonnenburgs have studied.
Perhaps each of these illnesses has a unique cause, or perhaps, as the Sonnenburgs surmise, they arise from a common root—the loss of a fundamental part of our ancient biology. “If you think of it, the microbiota is like an organ,” says Erica Sonnenburg, a senior research scientist at Stanford. “It’s this collection of cells that’s performing an important function in our gut. If you found out a third of the cell types in that organ were all of a sudden gone, it would be worrisome.”
The Good Gut, One Way Or Another
The Sonnenburgs go to great lengths to keep their own microbiomes in fine fettle. In 2015, they published The Good Gut, a layman’s walk through the science of the microbiome with plenty of real-life tips. The book included fiber-rich recipes rife with fermented ingredients and suggestions for a less zealous sense of hygiene than what Madison Avenue sells.
“The next time your infant sticks a new object into his or her mouth, if it is not a choke hazard, instead of rushing to pull it out or clean it with a sanitizer, consider how the bacterial patina is providing valuable microbes to help form the new microbiota,” they write.
They walk the walk. The family hand-mills its own wheat flour, brews beer with live cultures, bakes bacteria-leavened sourdough, favors fermented food and, of course, eats heaping amounts of fiber in a heavily plant-based diet. But in most cases, they acknowledge, we owe our microbiomes—as individual as our fingerprints—to circumstance. Justin Sonnenburg likens the formation of the average microbial community to Plinko, a contest on The Price Is Right game show, in which a contestant drops a disc into a maze and watches it fall. Sometimes it lands in the $10,000 spot and it’s all smiles; sometimes it’s $0 and tears. Either way, the result is random.

‘The next time your infant sticks a new object into his or her mouth . . . consider how the bacterial patina is providing valuable microbes to help form the new microbiota.’
But what if it’s possible to assemble a model microbiome that could be administered in early childhood, the time of life when our microbial community is most plastic? “The idea is, instead of letting the Plinko chip fall down the board, you walk up there and you put it into the slot that has the optimized health and immunity and metabolic trajectory for an infant,” Justin Sonnenburg says.
Poop That Heals
While it’s still a distant goal, the idea of programming someone’s microbiome is an alluring prospect with powerful precedent. In fact, one of modern medicine’s advances toward that aim—the fecal microbiota transplant (FMT)—resembles centuries-old Chinese and Bedouin remedies. FMTs use healthy donor poop to reseed the gut of a diseased recipient via such methods as ingesting “crapsules.”
In the West, the therapy existed mostly on the periphery, used by veterinarians, folk healers and mavericks. In 1958, the late Stanley Falkow, who would go on to become a revered professor of microbiology and immunology at Stanford, was fired from his position as a hospital technician for giving fecal pills to patients suffering from postsurgical diarrhea.
“Falkow, is it true you’ve been feeding the patients s**t!” an irate chief administrator at the New England hospital said before sacking him temporarily, Falkow wrote in 2013.
But the “yuck factor” ebbed as microbiome research bolstered the rationale for the practice. And FMTs have proved stunningly successful in treating C. difficile, a stubborn disease that arises in patients whose gut microbiomes have been laid low by antibiotics, allowing a weedy pathogen to take root. The disease causes debilitating, even deadly, diarrhea that’s often highly resistant to conventional treatment.
When Dutch and Finnish researchers undertook the first randomized, controlled trials of FMTs in treating the disease, reported in 2013, more than 90 percent of patients were cured. The results were so persuasive that the trial ended early. It also raised hopes of using such transplants for other diseases, like colitis and autism, which are similarly associated with damaged microbiomes. Yet, so far, this has not proved as fruitful. Herein lies a big “chicken-or-egg” question for microbiome researchers: Is a distressed microbiome always the cause of disease, as in C. difficile, or is it sometimes a symptom?
FMTs also present other challenges, including establishing that donated stool is pathogen free. Bhatt, for one, says she wouldn’t take the risk of transferring a thousand foreign bacteria into one of her immunocompromised patients.
Michael Fischbach, an associate professor of bioengineering, is considering a more targeted approach to tweaking the gut. He got his start studying microbes in the soil—they exist essentially everywhere—in search of genetic sequences associated with biosynthetic processes, including those that make antibiotics.
While scanning genetic databases, he found that some of the most promising gene clusters were not found in dirt but rather in people—in the microbes of their skin, mouths and guts.
Indeed, some of our gut bacteria are like little drug factories. A single strain may be capable of making up to 200 milligrams of a chemical a day, Fischbach recently told Stanford Medicine—the same amount of active ingredient in an Advil.
In certain cases, that’s good; in others, bad. Some people, for example, have a type of bacteria that converts a chemical common in red meat into a compound associated with heart attacks. A meat lover with that problematic bacteria could be more likely to develop heart disease than another person eating the same diet. Fischbach and others are investigating whether they can alter certain strains of bacteria to eliminate the dangerous traits, then reintroduce them back into the gut.
Is This Crap?
Tempering the many hopeful voices surrounding applications of microbiome research is Jonathan Eisen, PhD ’97, a professor at UC-Davis’s Genome Center who cautions against “microbiomania.” For years he gave out regular Overselling the Microbiome awards on his website, though he’s lately stopped. “It was too easy,” he says.
Despite his skeptic’s badge, Eisen is actually bullish on microbiome research. He believes the microbes that live in and on people contribute more to human health and well-being than we can currently show, but he says that with an emphasis on “show.”
“Yes, the microbiome is almost certainly involved in allergy, asthma, obesity, all sorts of inflammatory conditions, gut health and everything up to behavior, but just because someone has suggested or shown that doesn’t mean we have any idea how to work a correction for changing the microbiome to change any of those traits,” he says.

‘That day may come when we have devices in our toilets—they’re giving us a readout of what is going on in our microbiome.’
Justin Sonnenburg agrees that microbiome research is still in its toddler years. He, too, is concerned that runaway hopes could lead to the same disappointment that followed the slow pace of advances resulting from the Human Genome Project, which sequenced the entire human genome. It was a wondrous advance, but it failed to meet some people’s inflated expectations for immediate applications.
It may turn out that, for most people, the greatest benefits of the microbiome research come from heeding old wisdom for newly discovered reasons—like eating fibers and fermented foods to nurture good bacteria. A high-fiber French fry that tastes as good as a traditional one could do wonders, Sonnenburg says.
Still, individualized treatments could come to pass, he says, citing an Israeli start-up that can analyze your microbiome from a stool sample to predict how your blood-sugar levels respond to different foods. One person’s might spike after he eats a banana but not a cookie, a distinction with ramifications for health and athletic performance. The company doesn’t know the mechanics of why this happens. It relies instead on collecting enough information from enough people to make predictions based on correlation rather than causation.
The practice presages an increasing dialogue between us and our gut, via a humble intermediary. “That day may come when we have devices in our toilets—they’re giving us a readout of what is going on in our microbiome,” Sonnenburg says. “You can imagine a time in the future where you, as individualized and different as you are from everybody, will have an algorithm that understands how your gut microbiota respond.”
Sam Scott is a senior writer at Stanford.