"YOU KNOW THAT FEELING when you're digging through an ice cooler and it's so cold it's burning?" asks Sandra Hyde, a marketing consultant from Florida. "That's what my hand and foot feel like every day, all the time." Nearly 10 years ago, when she was just 20 years old, Hyde's right ankle was shattered in a car accident. The bones healed, but the pain never left. Her foot became discolored and swollen. Then the sensation spread, eventually affecting most of her right side, including her leg, arm, shoulder and parts of her neck and face. "It's never ending," she says.
For unknown reasons, complex regional pain syndrome, as Hyde's condition is known, occasionally sets in following trauma or surgery. It is just one manifestation of the body's vital protection system malfunctioning.
"Pain is our absolute most important sense," says assistant professor of anesthesia Jarred Younger. It signals bodily damage and drives a person to flee from harm or rest a mending injury. Babies born without the ability to feel pain due to a rare genetic disorder generally don't live past childhood. Such individuals unwittingly break bones, bite through their lips and tongues and let infections fester.
But when pain outlasts its evolutionary purpose it can be devastating, too. "When pain becomes persistent, it can become a disease in its own right," says Sean Mackey, chief of the division of pain management at Stanford Medical Center and a professor of anesthesia.
Though definitions vary, the term "chronic" is generally applied to pain lasting longer than six months. Several recent surveys have estimated the prevalence of chronic pain among adults in the United States to be around 30 percent. These figures encompass conditions like Hyde's, as well as more common varieties—arthritis, unremitting back and neck pain, and recurrent migraines—that nevertheless take a profound toll on daily life.
When standard analgesic medications fail to adequately manage a patient's symptoms, doctors may reach for powerful opioids such as Vicodin. But these drugs have serious drawbacks. Over time, patients require higher and higher doses to achieve the same effect, which can lead to addiction and/or overdose. More Americans are now dying as a result of prescription opioid overdose than from cocaine or heroin overdose.
In addition to the cost in human suffering, chronic pain costs the United States more than half a trillion dollars annually in direct medical expenses and lost productivity, according to a 2011 Institute of Medicine report (chaired by former School of Medicine dean Philip Pizzo). This is more than the cost of heart disease and cancer combined.
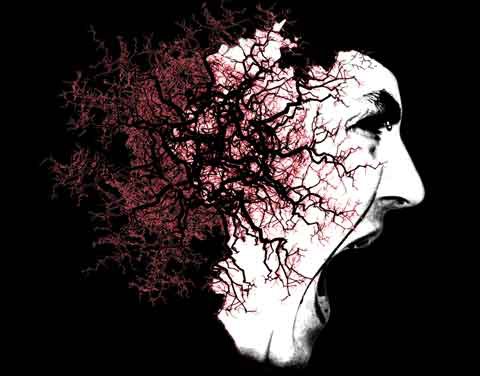
Traditionally, pain has been viewed as a symptom of something else rather than as a problem in itself. But increasingly Mackey and others believe that, like heart disease or cancer, chronic pain involves specific, measurable—and potentially treatable—abnormalities in the body. Mounting evidence from several labs at Stanford suggests that regardless of the initiating injury, chronic pain involves telltale changes in the brain, spinal cord and possibly the immune system. These insights are fueling the development of incredible new treatments that target these areas,rather than the place where it hurts.
PART OF THE DIFFICULTY of dealing with pain is that it's not just physical. Negative emotions such as anxiety and despair attached to bodily sensations are what make pain painful. This makes it a wily subject to study, as two people exposed to the same noxious stimulus can report vastly different levels of discomfort. It also suggests that there may be some truth to the adage that pain exists mainly in the brain.
At Stanford's Lucas Center for Imaging, researchers strap a probe to volunteers' palms while an MRI machine scans their brains. The probe feels hot, like it's burning the skin, but in reality the experiment is carefully controlled to avoid any actual damage or undue distress to the participants. Sensory receptors in the hand fire off urgent missives—Ouch!—which nerves in the spinal cord carry to the brain. There, the incoming signals rapidly engage multiple brain regions: not just sensory centers, but emotional and cognitive ones as well. "In an fMRI, you'll see most of the brain working on the pain in some way," Younger says.
Typically, once a danger has passed or an injury mended, the messages stop coming and activity in the brain subsides. But occasionally something goes awry. Across all types of surgery, one out of 10 patients will develop persistent pain after the wound has healed. For some types of surgery the rate is higher: 20 percent of patients who undergo knee replacement surgery develop chronic pain. What causes the circuits in some people's brains to become pathologically overactive remains unclear.
Neuroimaging studies from several different labs examining diverse types of pain offer tantalizing clues. They all show that chronic pain patients have stronger connections among brain regions involved in pain perception and processing, as well as losses in gray matter in those areas and perturbations in brain chemistry compared to healthy individuals.
These changes are so profound and consistent that a computer can be trained to spot chronic pain patients by their brain scans alone. In 2011, Mackey's team demonstrated just that. They taught a computer to recognize the brain activity pattern of a person experiencing acute pain. In 2012, they extended the work to chronic pain. When they fed structural MRI pictures from patients with lower back pain and healthy controls into a computer, it was able to distinguish these groups with 76 percent accuracy, based largely on gray matter changes.
Working with colleagues at Lucas, Mackey, who has a PhD in electrical engineering, also perfected a technique to obtain functional imaging scans of the spinal cord (tricky because the spine shifts with every breath). At a 2013 conference, his team presented preliminary evidence of amped-up connections in the spinal cord—which is responsible not only for routing messages to the brain but for sending inhibitory signals back to the body—that may play a role in chronic pain.
These technologies are not intended to replace a patient's subjective report of pain, typically rated on a scale from zero to 10 (10 being the worst agony imaginable). But the ability to detect and quantify pain objectively could prove useful in situations where patients aren't able to say how much it hurts. Moreover, it lends support to the view of chronic pain as a disorder of the central nervous system. And if researchers can locate pain in the brain, it means that doctors may be able to treat it there.
ONE BRAIN REGION of particular interest is the anterior cingulate cortex, thought to be responsible for pain's psychological component. When the ACC is removed or injured, people report that they can still feel the physical sensation of pain but that it doesn't bother them. Conversely, negative thoughts and emotions can lower a person's pain threshold, causing them to experience a given stimulus more intensely and creating a vicious feedback loop.
Physicians have long recognized that mind-body practices such as meditation, cognitive behavioral therapy and stress reduction techniques can help break this cycle. But these interventions affect the brain broadly and nonspecifically. What if, Mackey wondered, pain sufferers could be taught to modulate the activity of their ACC. "We wanted to know if people could develop learned control of that region and pump it up like a muscle, like sending you to the gym to work out your biceps."
He teamed up with an entrepreneur who had developed software to render fMRI images instantaneously—a process that previously took hours. The technology makes it possible for an individual to be shown his or her own brain activity in real time while in the scanner. To test the setup, members of Mackey's team applied hot probes to the arms of volunteers while they watched an image of fire displayed on a screen. The height of the flames represented blood flow to the ACC.
The volunteers were instructed to try to subdue the flames using a variety of mental strategies: equating them with a warm bath or visualizing a tranquil beach. Over the course of six sessions, eight subjects shown images corresponding to their own ACC activity learned to quiet the fire. Their ratings for the unpleasantness of the experience decreased 38 percent on average. Control subjects shown sham feedback—information from a different brain region or another subject's fMRI—had no benefit.
In a small pilot study using this real-time fMRI therapy, eight patients reduced their chronic pain an average of 64 percent. One of them, Melanie Thernstrom, wrote a book in which she describes the experience. "It was very empowering because it gave me this sense that I could control my brain," she says. In her case, thinking of calming scenes actually made her ACC activity flare; imagining that she was a martyr burning at the stake squelched it.
Mackey's team recently received a $10 million grant from the National Institutes of Health to test real-time fMRI therapy (as well as other mind-body therapies, including cognitive behavioral therapy) in a large randomized trial of patients with chronic lower back pain. The technology has evolved since the first study was published in 2005; volunteers now learn to control multiple brain areas, patterns of brain activity, connections between brain systems and even pain pathways in the spine.
ONE MIGHT EXPECT a pain lab to resemble a medieval torture chamber, but the lab where Kevin Johnson works is actually quite civilized. There are snacks on the table, a comfortable chair for volunteers to sit in and a smattering of innocuous-looking electronic equipment.
Johnson, a research associate in anesthesia, is demonstrating the potential of a technology called transcranial magnetic stimulation to precisely target and alter activity in specific areas of the brain. He holds the device—which consists of a wand fixed to two pancake-sized magnetic coils—over his head, aimed at just the right spot in his motor cortex to make his fingers twitch. He moves it slightly and his leg jerks. It's both eerie and fascinating to watch.
The magnets induce weak electric pulses that pass through the skull and alter the firing of nerve cells. More than a decade's worth of research has shown that repeatedly zapping the prefrontal cortex can affect mood, and in 2008 the FDA approved TMS for the treatment of major depression. Many patients treated over a four- to six-week period report fewer symptoms for months afterwards. "What that tells you is that you're actually causing structural changes—you're either strengthening or weakening connections in the brain," says associate professor of anesthesia David Yeomans.
Traditional TMS can only reach superficial areas of the cortex, though. So Yeomans is testing a novel four-coil system that can aim electric fields deep into the brain. His team uses sophisticated mathematical modeling to figure out exactly how to angle the magnets to hit specific brain structures, such as the ACC.
To validate that their models were on target, the researchers tested four different configurations of the multi-coil TMS on 19 healthy volunteers. Following 30 minutes of treatment with the device, a hot probe was applied to each volunteer's arm for 10 minutes while his or her brain was scanned using positron emission tomography (PET). For the most effective configuration, average pain scores went down 79 percent compared with a sham condition—from an average 5 or 6 out of 10 (relatively severe) to around 1 (minimal).
What's more, says Yeomans, "If you looked at the brain activity of the ACC under the sham treatment, it lit up like a Christmas tree; if we did it after the real treatment, it was greatly reduced."
In five patients with fibromyalgia, an enigmatic syndrome in which the lightest touch can be excruciating, the same coil configuration reduced chronic pain by 43 percent. The patients received multiple treatments over four weeks and the analgesic effect was maintained for at least a month, Yeomans says. "Which tells us that we are causing some kind of rewiring."
SOLVING THE MYSTERY of fibromyalgia has been a central theme of Jarred Younger's career. The disorder affects about 6 million Americans, predominantly women. The afflicted don't appear to have anything wrong with their muscles, joints or ligaments; yet even mild pressure can cause agony. Younger and others now suspect that fibromyalgia involves inflammation in the central nervous system. "We know that somewhere in the spinal cord or in the brain, normal messages are being amplified," he says.
When you get the flu, microglia cells in your brain and spinal cord pump out chemicals called cytokines—they're what make you feel fatigued, groggy and achy. "We think it does that to force you to rest, so your body can devote its resources to fighting off the infection," Younger explains. He believes that in fibromyalgia this system is pathologically engaged. "Their immune system has been tricked into thinking that there is a constant infection."
Daily fluctuations in certain cytokines correlate with patients' pain experiences, supporting this hypothesis. But whereas drugs such as steroids and ibuprofen are effective at reducing peripheral inflammation, they don't easily cross into the brain or spinal cord and are thus ineffective for treating inflammation in the central nervous system. In a 2013 study by Younger's team, 31 fibromyalgia patients treated with low doses of a drug called naltrexone that inhibits microglial cells in the CNS reported significantly less daily pain on average compared with a placebo pill.
The link between the immune system and chronic pain is an unfolding story that encompasses other types of chronic pain, including complex regional pain syndrome. David Clark, a professor of anesthesia who studies the condition, notes that some of its features—redness and inflammation at the site of the original trauma; other body parts becoming painful and disabled; the development of neurological problems—are reminiscent of autoimmune disorders.
Indeed, Clark has demonstrated inflammation beyond the originally affected limb in animal models of complex regional pain syndrome. Other researchers have shown that human patients have elevated levels of pro-inflammatory cytokines in their cerebrospinal fluid.
In Sandra Hyde's case, Sean Mackey prescribed a microglial inhibitor called dextromethorphan, which is available in over-the-counter cough syrup. "I could immediately tell the difference within a week of taking it," she says. "It's phenomenal." She needs smaller shoes because the swelling in her foot has finally disappeared.
Hyde, who flies cross-country for bimonthly appointments at Stanford, says she's also benefitted from working with a multidisciplinary team of specialists including a physical therapist, a nutritionist and a pain psychologist who meet with Mackey to discuss her case.
LIKE MANY CHRONIC DISEASES, pain can be managed, though rarely cured. But what if it could be prevented altogether? Assistant professor of anesthesia Ian Carroll and his team are investigating whether giving certain drugs immediately before and after surgery can prevent pain from ever gaining a foothold.
For example, gabapentin, an antiepileptic drug that dampens nerve firing, may keep pain messages from overwhelming the brain and spinal cord. And minocycline, an antibiotic that also acts as a microglial inhibitor, may prevent the development of central inflammation.
Carroll, who started his career as an anesthesiologist, says it was Mackey who hooked him on pain medicine. "Sean was convincing that if you were going to go into academic medicine and do research, the questions that needed answering were in pain."
Many of those questions remain unanswered, Mackey says. "We're practicing in the dark ages, maybe even the Neanderthal ages." But he's hopeful about the future: "Twenty to 30 years from now, we're going to look back and say: 'We fused spines? We gave medications that just flood the brain? Wow, that was pretty primitive compared with the treatments we have now.' "
Kristin Sainani, MS '99, PhD '02, is a freelance writer and clinical assistant professor in the department of health research and policy.